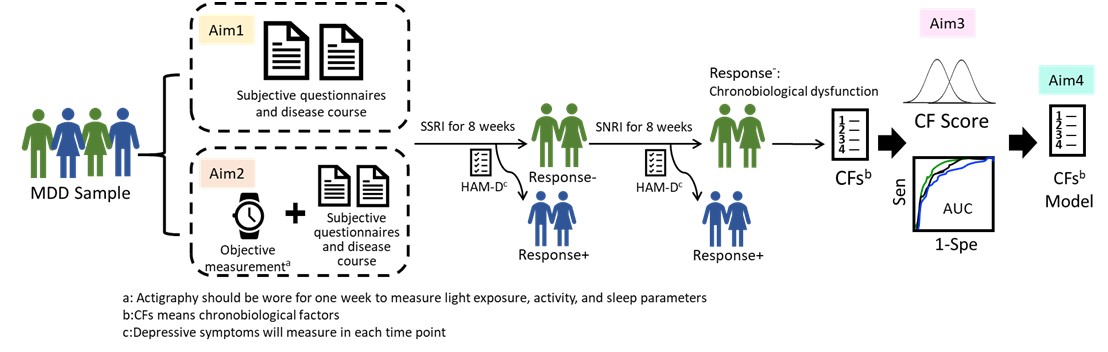
Major depressive disorder (MDD) is a sever and complex psychiatric disorder, with high frequency of episodic recurrence. Disease course chronicity often leads to cognitive and functional decline, and causes heavy economic and disease burdens. However, half to two-thirds of MDD patients do not respond fully to first line option of antidepressants treatment and often suffer from severe depressive symptoms or mild symptoms during partial remission. One of the main reasons is the phenotypic and etiology heterogeneity among MDD patients, and the limitation of current pharmacotherapy. Neurotransmitter imbalance has long been the center for drug discovery, such as selective serotonin reuptake inhibitors (SSRI) and serotonin noradrenaline reuptake inhibitors (SNRI). Recently, drug that targets on other system is also on the market. It is apparent that we need more sophisticated measures and clinical features refinement to assist dissecting heterogeneity in MDD, and in turn to benefit the selection of clinical regimen and treatment response in patients. Notably, substantial proportion of MDD patients exhibit features of chronobiological dysfunction, including ultradian, circadian, and infradian rhythms. Its related clinical characteristics often consist of insomnia, abnormal sleep patterns and sleep-wake cycle, irregular activity pattern, shift chronotype, hyper-sensitive to seasonal changes, etc. Although chronobiological dysregulation is quite common in MDD patients and contributes on the heterogeneity of MDD, it requires further study to quantify the magnitude of such dysregulation, and to identify representative core chronobiological factors (CFs) through different screening stages. There are plenty of aims in the current proposal. At the first stage, we will conduct a two-year observational study with guided treatment sequence (the order of drug treatment is SSRI, then SNRI) on MDD patients with acute episode. It is assumed that patients who do not response to serotonin-based treatment might have more pronounced chronological dysregulation. On the other hand, we also collect subjective and objective data for several assessments in different aspects of chronobiology, using approaches of interview and questionnaires for subjective part and Actigraphy to collect sleep parameters and daily activity data for objective part. These variables will be related to treatment response to obtain relevant subjective-based and objective-based CFs. At the second stage, we will integrate all the information and create a quantified CFs scores to weight the levels of chronobiological dysregulation for each individual. A prediction model can then be built-up using the CFs score for good and poor treatment response. At the third stage, patients can then be screened and quantified for their chronobiological dysregulations using pre-set CFs score cutoff. After that, we will validate the results between CFs score and the real treatment result. We anticipated that results of this proposal would enhance our understanding for the contribution of chronobiological dysregulations in the heterogeneous MDD patients and can benefit treatment outcomes at earlier stage by improving treatment regimen in clinical setting in the near future.